For the first time, Australians with type 2 diabetes not using insulin will have access to blood glucose monitoring (BGM) strips restricted. Jayne Lehmann continues with the second instalment of a blog that guides Credentialled Diabetes Educators (CDEs) and health care professionals through the new guidelines and their implications for people with type 2 diabetes. Tips to support people with diabetes through the changes are included.
Structured BGM
Quality information with less blood glucose monitoring (BGM) is the focus for people with type 2 diabetes not using insulin and their health professionals as the restrictions come into effect on 1st July 2016.
CDEs are the experts in structured self BGM. Structuring BGM for quality results rather than quantity means less strips, less finger pricking pain and more involvement by the person checking, thinking about and acting on their blood glucose levels.
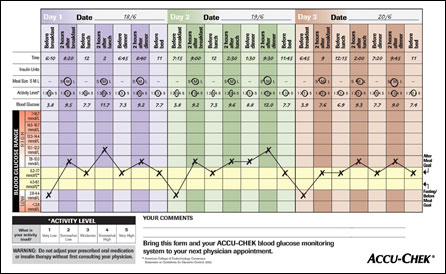
Paired testing (checking levels pre and 2 hours post meals) and structured monitoring (either rotating times pre and 2 hours post meals or 3 consecutive days of BGM pre and post each meal and before bed) supports a comprehensive review of the impact of food, exercise, stress and medication. Once stabilised the person has a break from monitoring.
Greater return for investment in BGM strips is achieved if you get the person to …
CHECK their blood glucose levels at the right times
… THINK about their number and if it is in or out of their target range
… ACT on the results to get their numbers back in range.
Some people will need to be weaned from their reliance on BGM if their levels are well controlled and clinical need does not indicate eligibility for a further 6 months of strips.
Tip: Tell people what their target levels are before and 2 hours after meals and the actions they need to take if high or low. I have designed a handout, the Check, Think and Act© that supports the person to Check, Think and Act on their diabetes numbers for good health.
Tip: Stock up on structured BGM tear-off charts like the one above and give people with type 2 diabetes not using insulin a number of copies. Demonstrate their use and encourage completion of the 3-day profile before their next appointment. Evaluate their use of the tool, provide more education if required and review levels. Once stable, regular BGM can be put on hold and paired testing used to investigate impact of food portions, exercise, stress or medication on glucose levels. A 3-day profile is completed prior to their next diabetes care review appointment with the CDE, doctor or nurse practitioner.
Interpretation may cause conflict
The Choosing Wisely campaign and the RACGP’s GP Diabetes Management Guidelines (18th edition) endorsed the recommendation:
Don’t advocate routine self-monitoring of blood glucose for
people with type 2 diabetes who are on oral medication only
There is potential for a clash of opinions between health professionals who interpret the recommendation as “people with diabetes not on insulin don’t need to monitor” vs. “people with diabetes not on insulin need to structure their monitoring”.
The inclusion of CDEs as signatories on the NDSS assessment of clinical need forms has acknowledged the role we play in supporting people to be actively involved in their diabetes care. We have been given the authority to review clinical need for BGM. Documentation of the assessment, implementation and evaluation of our review for clinical need in each individual will be essential. So too a communication process with the GP to prevent confusion.
Tip: Review the research underpinning structured BGM and note some appropriate references to include in letters back to the doctor if required. Document your assessment and recommendations and include a summary in letters back to the doctor. Talk to the person with diabetes about the wording of the guidelines and highlight structured BGM is not a routine approach.
Potential risks
The glycosylated haemoglobin (HbA1c) is said to be the ‘gold standard’ in the assessment of diabetes care. People who are unable to check their blood glucose levels due to the new guidelines become more reliant on their HbA1c results. There is a potential risk in this strategy if HbA1c results are adversely affected by other co-morbidities. Table 1 summarises conditions that can cause HbA1c inaccuracies (RACGP Diabetes Management Guidelines (18th Edition) Section 8.1 Glycaemic Monitoring and Control).
| Table 1: Conditions associated with abnormal glycosylated haemoglobin (HbA1c) | |
|---|---|
| Abnormally low HbA1c | Abnormally high HbA1c |
| Haemolytic anaemia | Iron deficiency anaemia |
| Haemoglobinopathies | Splenectomy |
| Acquired haemolytic anaemias (e.g. drug-induced such as dapsone, methyldopa) | Steroid therapy, stress, surgery or illness in the last 3 months |
| Recovery from acute blood loss | Alcoholism |
| Chronic blood loss | – |
| Chronic renal failure (variable) | – |
Usually a discrepancy between the glycosylated haemoglobin (HbA1c) and BGM readings will be the alert of a problem with HbA1c accuracy. Fructosamine testing is more accurate as a long term parameter if co-morbidities exist.
Tip: Print and keep Table 1 as a ready reckoner on conditions that affect HbA1c accuracy and recommend fructosamine testing if any exist. Those without a co-morbidity, use extra vigilance in checking HbA1c and BGM correlates during periods of blood glucose monitoring.
Tip: Print and keep Table 1 as a ready reckoner on conditions that affect HbA1c accuracy and recommend fructosamine testing if any exist. Those without a co-morbidity, use extra vigilance in checking HbA1c and BGM correlates during periods of blood glucose monitoring.
Is there a possibility the Legacy Effect identified in the UKPDS follow-up studies will be diluted if BGM is not available early in the diabetes journey to achieve diabetes targets?
What constitutes clinical need to approve strips?
The introduction of restrictions to access BGM strips will focus CDEs, doctors and nurse practitioners on clinical need for BGM. Table 2 lists the Commonwealth government’s criteria for assessing people with type 2 diabetes not using insulin treatment and examples that fulfil the criteria to access strips.
| Table 2: Assessment criteria re clinical need for SBGM in type 2 diabetes/no insulin | |
|---|---|
| Criteria | Examples of clinical need for SBGM |
| The person has an inter-current illness that may adversely affect blood glucose control | Iron deficiency anaemia |
| Haemoglobinopathies |
|
| The person is undergoing treatment with a medicine that may adversely affect blood glucose control |
|
| The person’s diabetes is inadequately controlled |
|
| Clinical need for the person to self-monitor blood glucose control |
|
| There has been a change to the person’s existing diabetes management within the previous three (3) months. |
|
1st of July 2016 marks the beginning of a significant change in the use of BGM strips by Australians with type 2 diabetes not using insulin. CDEs are the experts in structured blood glucose monitoring. Their ability to focus people with diabetes to Check, Think and Act on their diabetes numbers provides quality BGM. Get in touch with your local GPs and highlight how you can support people to understand the restrictions and authorise strip access and capitalise on this opportunity for increased referrals.
Want to know more?
- See more of Jayne Lehmann’s blogs: www.edhealthaustralia.com
- National Diabetes Services Scheme: https://www.ndss.com.au/important-changes-to-the-ndss
- Diabetogenic blog by Renza Scibilia State of Health https://diabetogenic.wordpress.com/2015/06/01/state-of-health/Choosing Wisely not so Wise at All https://diabetesaustraliavic.wordpress.com/2015/04/30/choosing-wisely-not-so-wise-at-all/
- Blog – Type 1 writes by Frank Changes to the NDSS from 1 July 2016
http://www.type1writes.com/2016/04/13/changes-to-the-ndss-from-july-1-2016/ - PBS Post Market Review of Products used in the Management of Diabetes http://www.pbs.gov.au/info/reviews/diabetes
- The Royal Australian College of General Practitioners (RACGP) 18th Edition of the General Practice Diabetes Management guidelines http://www.racgp.org.au/your-practice/guidelines/diabetes/
- Choosing Wisely RACGP tests, treatments and procedures clinicians and consumers should question http://www.choosingwisely.org.au/recommendations/racgp


