CGM – A game changer in understanding a person’s diabetes

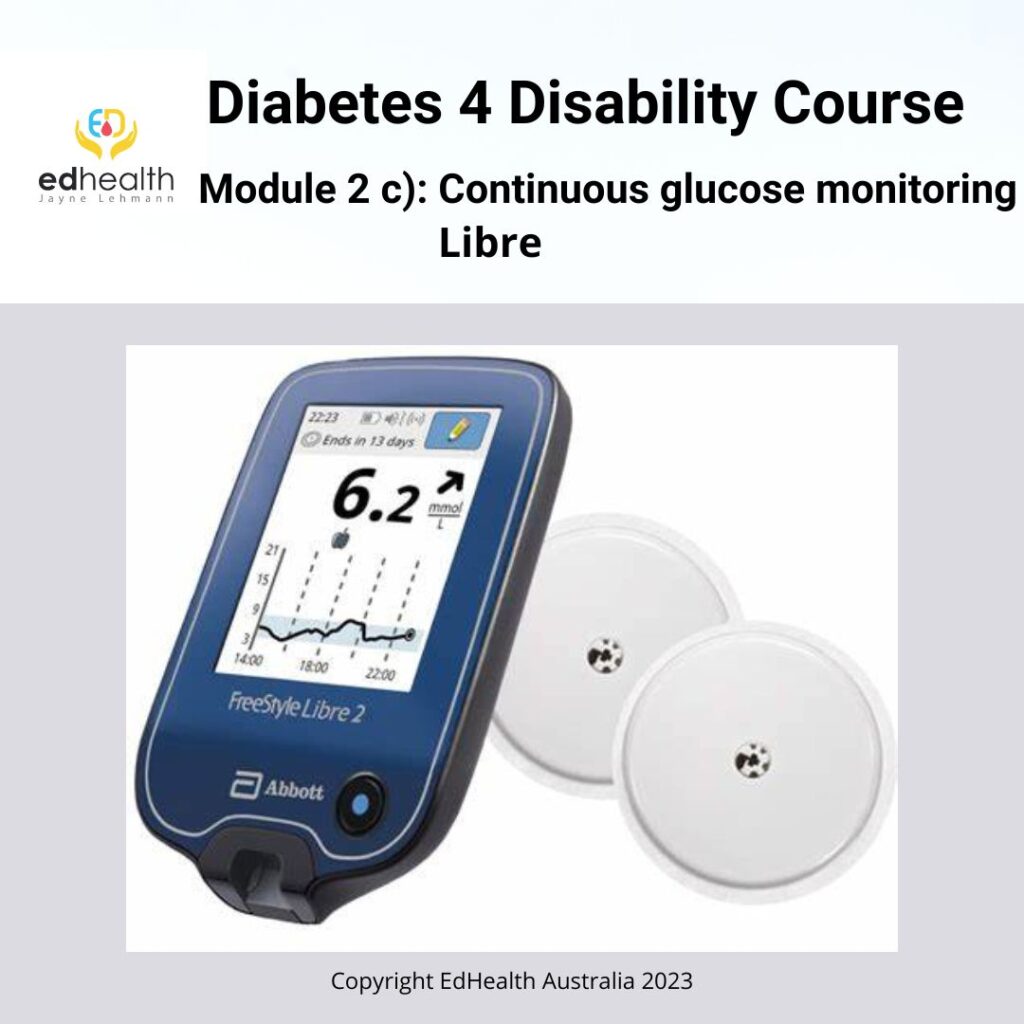
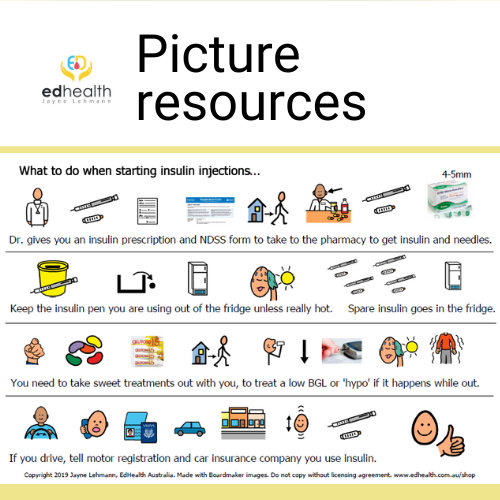
People with diabetes need to know what their glucose levels are doing to take good care of their diabetes. When you also have a disability, technology, like CGM, can be the answer to being able to help you to keep your glucose levels on track for good health. Their claim to fame is the ability to check glucose levels without pricking a person’s finger for a drop of blood. Instead, a sensor is inserted into the skin, to record the amount of glucose in the fluid around the cells, every five minutes. Wi-fi lets the readings move, via Bluetooth, to an App on a Mobile phone, or Reader.
All people with type 1 diabetes can access subsidised CGM in Australia
The advantage of CGM is that will/is:
- Record lots of readings over twenty-four hours, including overnight
- Easy to see the impact of food, activity, stress and medication on glucose levels
- Able to pick up patterns in the readings to inform medication changes
- Improved evaluation of medication prescribing, de-prescribing and dose changes
- Pick up low readings earlier using the alarms; for highs, lows and when dropping quickly.

The National Diabetes Services Scheme (NDSS) provides all Australians with type 1 diabetes with access to subsidised continuous glucose monitoring via the National Diabetes Services Scheme for people over 21 years of age.
People with type 1 diabetes and an intellectual/cognitive or psycho-social disability have the same access to this program as a person without a disability. The CGM equipment is all accessed via the NDSS – It is not covered by the National Disability Insurance Scheme (NDIS) for people with type 1 diabetes.
It is important for people with intellectual disability to be actively considered for the use of these technologies. The NDSS provides the equipment at a significant subsidy and having an intellectual disability or other significant disability is not a reason to exclude their access to this equipment. The information gained from the readings makes it possible to comprehensively review insulin and lifestyle (food, exercise and stress) management to work towards keeping their glucose levels in the healthy range for longer (this is called ‘time in range’). They feel better day-to-day and gain some protection from sudden, very low and very high glucose levels. The setting of well-considered alarms is likely to increase time in range because of the earlier alert when readings drop quickly, or it gets close to being too low, or hypoglycaemic (hypo). In these circumstances, a snack eaten when their glucose level is slightly higher is likely to stop the readings from dropping into the hypo range.
Click! for more information about CGM and the NDSS.
People can choose the type of equipment they want to use through this scheme. For NDIS participants, the EdHealth clinical team can give you some advice on equipment to suit your needs best. Otherwise, talk to your endocrinologist or diabetes educator.
Click! to find out more about the CGM equipment available from the NDSS.
What if I have a disability, type 2 diabetes and use insulin?
People with type 2 diabetes are not eligible to get the CGM technology via the NDSS. Only people with type 1 diabetes. If a person with a disability is not able to do blood glucose monitoring due to the impact of their disability, they may be eligible to apply through their NDIS Plan to have the CGM funded.
EdHealth has considerable experience providing an assessment and report to argue for the funding of CGM systems by the NDIS for people with a disability eligible for this funding. The NDIS requires there to be an assessment and a report outlining the reasons for the recommendation and how it is linked to their disability. Once funded, EdHealth can also provide staff/client training and write a Diabetes Management Plan to guide the support to be provided by the support workers.
Barriers to blood glucose monitoring for people with a disability
People living with intellectual, cognitive or psycho-social disability, CGM may face barriers and are not able to check their blood glucose levels enough, or not at all.
Barriers may include:
- Challenging behaviour triggered
- Fear of blood or finger pricking
- Finger/hand/arm malformation or amputation
- Finger prick refusal
- Loss of hand or arm function.
- Painful finger pricking causing sore fingers
- Peripheral neuropathy and at risk of infection in fingers if finger pricking.
- Support workers not trained to do blood glucose monitoring
- Vision loss.
EdHealth’s Diabetes 4 Disability Program
The Diabetes 4 Disability(D4D) program includes 13 individual services. NDIS participants can have one of the EdHealth team assess the disability side of their capacity and ability to self-care for their diabetes. We design a person-centred solution, using D4D services hand-picked, individualised and wrapped around the individual. This sets up the person and their circle of support for quality, safe and effective diabetes support.
EdHealth trains support workers to put in the sensors, understand how the system works and to know what to do with the records generated by the system. We also recommend an individualised Diabetes Management Plan


Click! to find out more.
Copyright 2023 EdHealth Australia – improving diabetes health and wellbeing through education and innovation

